How to get a handle on your parent's meds
Your parent probably takes more medications than you realize.
My father was 75 the first time he was discharged from a skilled nursing facility, and I did a lot of things to try to ease his reentry.
I started managing his medications, taking each pill and placing it into either the “morning” or “evening” section of his rainbow-colored, day-of-the-week pill organizer. I sometimes dropped the pills or forgot which ones to split using the blue pill splitter. I squinted at the labels, checking how many pills were needed, how many times per day, and Googled what the medications were for. I couldn’t imagine him having the patience (or the vision) to do this himself. I didn’t know until much later that some experts don’t recommend using a pill organizer like the one we had—it’s harder to track exactly which medication you’re taking when they’re not in their original bottles and one error is easily repeated for seven days.
Eventually, my dad found a pharmacy that not only delivered his medications each month but also supplied them in blister packs labeled with the date and “morning,” “evening,” and “bedtime.” This took a task off my plate and made his medication process safer, in theory.
Reality was a bit different. My dad had unusual sleeping hours. He’d often stay up all night and doze off in his recliner between 4-7 a.m. Then, if he had nowhere to be, he’d sleep until late in the afternoon. So was he supposed to take his “morning” medications when he got up? Was he supposed to take his “evening” medications right before going to bed? When, then, should he take the “bedtime” meds? What if he never “went to bed” and instead just nodded off while watching movies in the living room?
When I cleaned out his apartment after he died, I found medication everywhere. Blister packs of meds he hadn’t taken while he was in the hospital, pill bottles for meds that hadn’t made it into the blister packs for some reason, blister packs he’d missed, and lose pills under the chair, in the trash can, and in the drawer of the table beside his recliner.
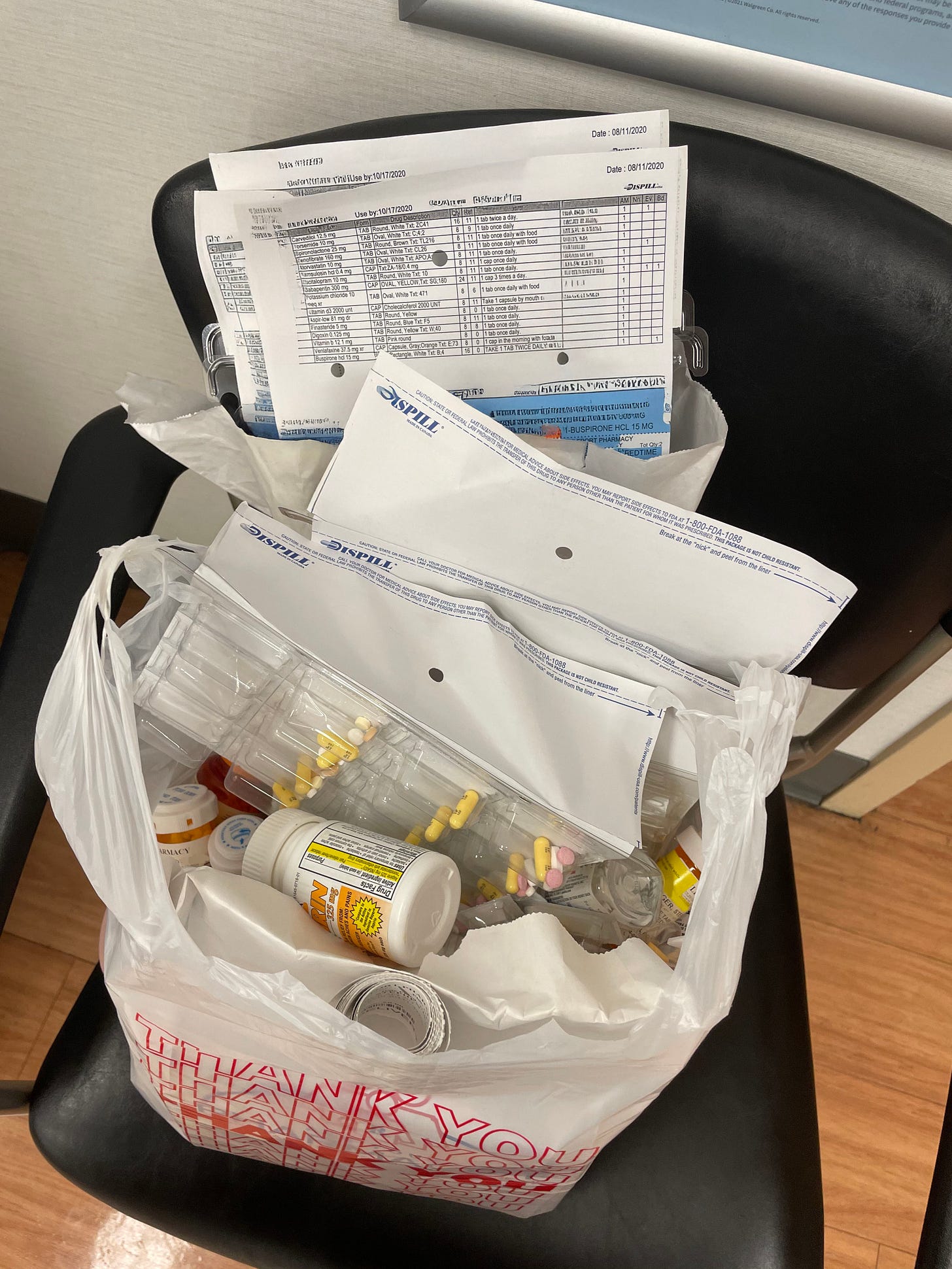
When we went to doctor’s appointments, I always brought the list that came with the medications, or, before that, a breadbox full of pill bottles. I listed off each medication, asked what it was for, and questioned whether it was the right one to continue.
Your parent likely has more than one health care provider. My dad saw a primary care doctor, cardiologist, cardiac surgeon, nephrologist, dermatologist, ophthalmologist, and urologist. In a perfect world, each provider has a full picture of the medications and treatments all the other specialists have prescribed, but if not, you might need to provide the information to bridge this gap.
Tips for helping your parents manage their many medications:
Bring medications to every appointment.
I often brought the whole breadbox of pill bottles to appointments, especially if I thought something was off with dosage or timing. Don’t worry about looking weird; much better that you feel awkward pulling out bottle after bottle than your parent take the wrong medication. My dad was often taking more than a dozen medications, plus supplements of vitamins and potassium. Bring everything. If you feel confident that each medication, including its dosage and timing, is on a list (in your Google doc or in their patient portal), bring the list.
Each time a new medication is prescribed, interrogate it.
If a provider is prescribing a new medication for your parent, check this list of questions and ask about interactions and guidance.
Beware “forgotten” medications.
Sometimes a past doctor prescribed a medication and your parent keeps them taking out of habit. Maybe it’s set to “auto refill” from the pharmacy and their current doctor is unaware. You need to make sure your parent’s current doctors are aware of everything they’re taking, including vitamins, gummies, and supplements. Especially if a specialist prescribes a medication or if something is added while your parent is in the hospital, be sure your parent’s primary care doctor knows about the addition.
Bring medications to the hospital.
If your parent is admitted to a hospital, bring the medications (or at the very least, a comprehensive list) with you if possible, and go over these medications with a nurse or doctor. They’ll administer their own meds there, but it’s helpful if they know exactly what he was taking at home. Every time my dad went into the hospital, he got off schedule with his antidepressants. If you live farther away from your parent, ask when you call in for updates if they have the most updated list of medications, and have them go through those with you on the phone as you cross reference with your own records.
Ask your parent about taking medications.
Do they take them at a set time each day? With food? How do they keep meds straight? Do they ever feel weird, dizzy, drowsy after taking their medications?
Do your own research on drug interactions.
Google “drug interaction checker” and lots of results will pop up for free sites that will allow you to add the drugs your parent has been prescribed and check whether there are troubling interactions. Even foods can interact with medications, like grapefruit juice. Each time your parent is prescribed a new medicine, do a little Google search and check for things like this. If you find something that doesn’t sit right with you, ask about it at the next doctor’s appointment you attend or encourage your parent to ask.
Don’t forget supplements.
When my dad went in for heart surgery in his 50s, as soon as they made the first incision, he began to bleed excessively. My mom said the OR nurse described it as a “blood geyser.” It turned out that he hadn’t disclosed that he was taking St. John’s Wort, which can interact with various heart medications and amplify the effects of blood thinners. Try to get the full picture of everything your parent takes, and revisit this conversation periodically.
Clear the medication clutter.
Check the expiration dates for medications that are used infrequently. Encourage your parent to ask whether a new prescription or new bottle of OTC meds is needed. Often, your parent’s health insurance will have an allowance for OTC meds. Help your parent properly dispose of old or unneeded medication. Most pharmacies have a safe box where you can dispose of old medications. People may look at you weird if you bring these in a huge shopping bag and it takes you 20 minutes to drop them all in (ask me how I know), so try to do this periodically instead of all at once.
Ensure meds are stored safely.
If you still have two living parents, or if someone else visits the home, it’s especially important to keep your parent’s medications in a safe place where no one will take them accidentally. Separate your parents’ medications, ensure they are out of reach to kids or pets but within reach of your parent. If children or teens, or other adults you don’t know well, frequently visit your parent’s home, consider getting a lockbox or a lock for a cabinet for your parent’s medications.
Be alert to your parent making changes.
Your parent knows best how they feel. Trust them when they say they don’t like a certain medication. If they indicate that they want to stop taking a medication, discourage them from stopping without first consulting a provider. Some medications can be dangerous to stop suddenly, and some can be easily transitioned to an alternative form (from a large pill to a liquid, for example). Help your parent identify the problem with the medication and facilitate a conversation with their doctor if necessary.
Be cautious when switching to a new system.
If your parent has been taking their medication a bit haphazardly, missing doses or entire days, it is possible that their provider has increased their dosage to unknowingly account for this. You can see how this would happen, right? “Hmm, you’re not feeling any better with 10mg, let’s try 20, okay?” And then if you switch to a foolproof system where they’re taking everything on time, it might be a bit of a shock to their system. Talk to your parent’s doctor before trying a new system.
Let’s learn from your mistakes
What mistakes have you made when it comes to your parent’s meds? Let me know in the comments if there’s a system that has worked (or definitely not worked) for your family.


Coincidentally, I decided I needed to get a handle on his medications a few weeks ago and he gave me holy hell, like I was treating him like a child/he has his system/he fills his organizer on Sundays… I insisted and wrote down each medication as he filled the little boxes on a list I (still) intend to type up (but haven’t yet.. nonetheless at his next appt, when the med tech started asking about medication, I was able to hand over that list and even though it was still the handwritten one, I have beautiful penmanship and the tech was grateful to peruse the list and my father didn’t have to pull out the ancient fold-up card he keeps in his wallet (which I’m sure is outdated). I felt organized, efficient, on-top-of-things.
But that was a few weeks ago. I don’t sit with him every week to fill up his organizer. I don’t ask him every day if he took his meds becuz that would only elicit anger.
It does feel like there’s a fine line between care and control. And with our aging parents, it’s so different than with our children. With my son, I am expected to slowly relinquish control as he embarks on his independence… allowing him to make mistakes whilst being a safe place for guidance and support. With my father, I am expected to… seek control without his wanting or asking for it, as he fights me every step of the way…? I can see some decline, some memory loss. But in the grand scheme of things, he is managing. I don’t know how to do this — I guess as things change/deteriorate, it’ll become obvious.
I do like your substack. I’m not going to lie, it does often make me feel guilty over mistakes I’ve already made, mistakes I’m likely making as we speak. But it’s good to read and feel a sense of normality—other people have been here before…
Thank you for writing.